By Emilie McKinnon

The second Editor’s Pick for September comes from the Institute of Health and Biomedical Innovation at the Queensland University of Technology (QUT) in Brisbane, Australia. We recently spoke with co-authors Monique Tourell and Konstantin Momot about why and how they used portable NMR to assess breast tissue density.
MRMH: First of all, can you tell us a little bit about your journey to MRI?
Monique: I did my undergrad studies at QUT (Queensland University of Technology) and did both my honors (a mini-masters) and PhD with Konstantin, using diffusion to study anisotropic structure in collagenous tissues. Then, while my PhD was being conferred, we worked on this paper together. Over the last year, I have been doing more fundamental NMR research at the University of Southampton and now I am back in Brisbane looking for my next project!
Konstantin: I am actually a physical chemist by training. I did my undergraduate studies in Russia, at Novosibirsk University, my PhD in Arizona with inorganic physical chemist Ann Walker, and my first post-doc in North Carolina at UNC with Charles Johnson (the inventor of DOSY-NMR). That was my first serious introduction to diffusion, and my research has since been connected to various aspects of diffusion, although it is actually not part of this paper [laughs]! I have now been in Australia for about 17 years where my work involves using MRI and NMR to deal with problems that have some sort of biomedical relevance.
MRMH: What are the take-home points of your paper?
Monique: Well, the main one is that the Mouse (the portable NMR probe) can be used to distinguish between low- and high-density tissue. We also found that the range of values seen across the patients could be attributed to different compositions in terms of fatty versus non-fatty tissue. Another take-home message is that the different regions could be determined just as well in the large breast slices as in the smaller segmented regions.

Konstantin: Yes, I would agree with that! This was a proof-of-concept paper in the sense that we demonstrated the use of portable NMR to distinguish between high- and low-density breast tissue. This study was done in vitro but it would actually be easy to extend to in vivo settings. In time, this technique could allow us to work not just with small excised portions, but also with large masses of tissue and still see what’s going on.
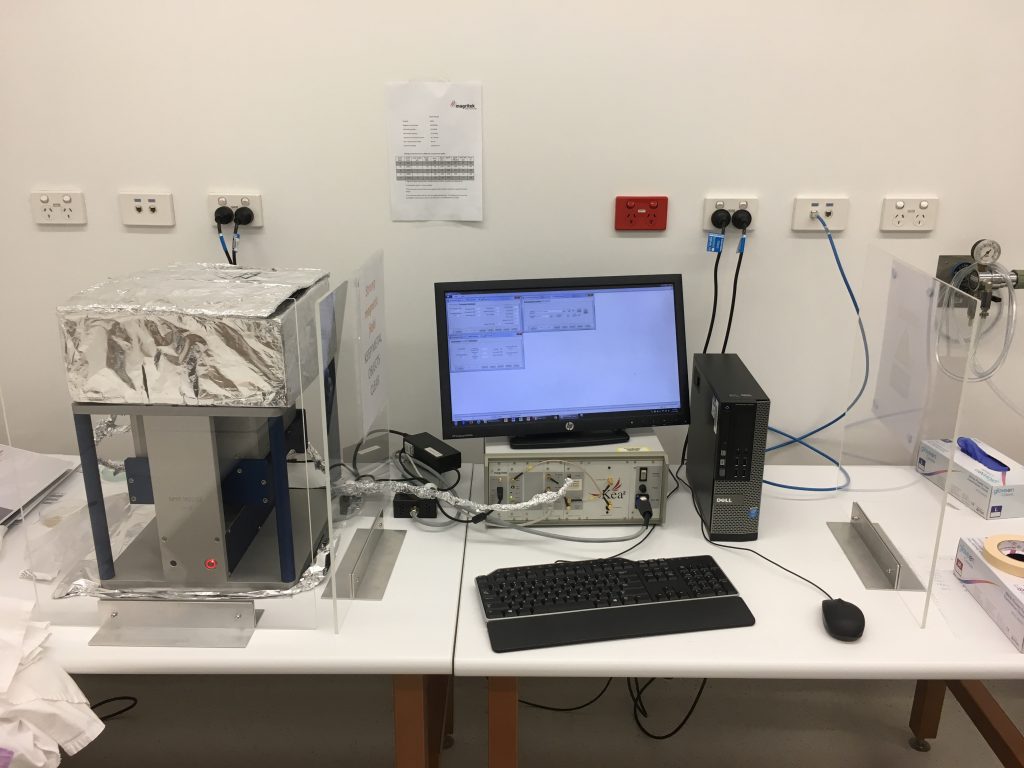
MRMH: Can you tell us a little bit about the hardware that was used for the experiment?
Konstantin: The first single-sided NMR sensor was made in 1996, I think. Back when it was invented it looked like a computer mouse, and was thus dubbed the “Mouse”! The hardware has undergone massive redevelopments since then, and now it just looks like a sort of rectangle. Basically, it’s a portable scanner with a permanent magnet, which you can move up and down to give you the depth profile. It costs only a small fraction of the cost of a full-blown MRI. Portable NMR is more of a sensing than an imaging technique and there is a definite niche in the clinical environment for this sort of instrumentation! After all, you don’t always need a laser, sometimes you just need a hammer!
MRMH: Why did you start with T1 as opposed to T2 relaxation, or ADC let’s say? Do you think these various NMR metrics could complement each other?
Monique: There are probably two reasons. The first is that T1 is more clinically relevant and is used more for imaging breast tissue because of its fat suppression capabilities. It was also just a simpler measurement for us to do straight up. It fits a mono-exponential curve, and so it was nice not to have to worry about issues like the distribution of different relaxation times or tissue orientation.
Konstantin: We have actually tried T2 and diffusion measurements as well! T2 brings out the composition differences in a slightly different way, and we expect T1 and T2 quantification to prove complementary. As another option, we could potentially ditch the idea of the recovery curve and explore approaches such as MR fingerprinting. Instead of a detailed image you can acquire a “fingerprint” based on the magnetization response of your sample and classify it as high or low density. This is one of the obvious avenues to pursue with portable NMR, especially seeing how successful MR fingerprinting has been in the brain over the last 2-3 years!
MRMH: One practical disadvantage of using NMR is that it would allow only a subset of the tissue to be explored. Do you foresee your technique being used in conjunction with mammography?
Monique: I see it as complementary to other spatially resolved techniques. It allows you to monitor changes in breast tissue more frequently, and then, if you spot something not quite right, you can go ahead and do a more detailed scan in that particular region, using MRI or mammography.
Konstantin: This is still an open question really, but I can see three basic scenarios. One of the problems with mammography is that it is a 2D projection technique being used to try and visualize a 3D structure. In this sense, portable NMR, allowing depth profiling, could be highly complementary. Another possibility is that we could select a number of certain strategic locations on the breast and use those as markers. The third scenario would be to use the technique for longitudinal monitoring of mammographic density, given that portable NMR is harmless and does not involve the use of ionizing radiation. There are certain treatments, such as hormonal treatment with tamoxifen (a breast cancer prevention drug), to which approximately 2/3 of patients respond. The major indicator of who is going to respond is the presence of early changes in mammographic density. From this perspective, longitudinal measurements are very useful clinically. In this setting, the same locations would be scanned each time.

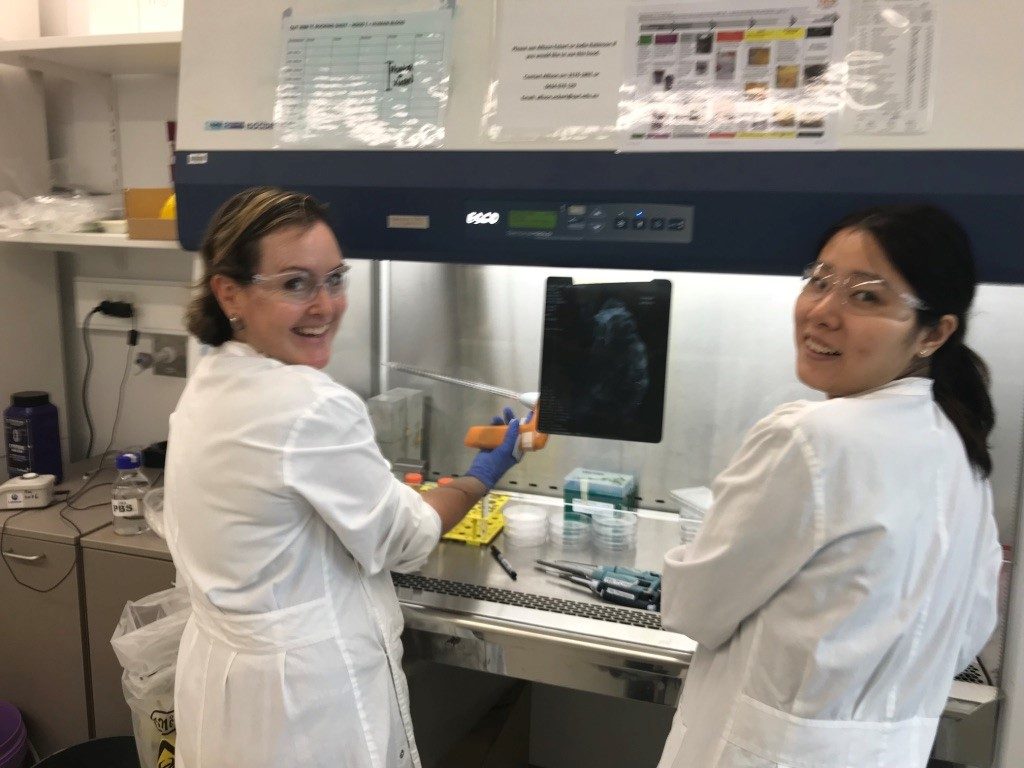
MRMH: This project seems to be a collaboration between many different specialties: pathologists, surgeons, radiologists and so on. What lessons did you learn from the clinicians that contributed to the successful completion of this project? What were the particular challenges you faced?
Monique: Communication is definitely a massive challenge when you are dealing with that many people! That said, I think clinicians are really good at keeping you focused on the clinical goal and what is actually relevant.
Konstantin: That was one of the lessons I learned as well. And I also came to realize that research involving actual patients takes a long time! We are used to working with in vitro samples, where things are easy. If you want to measure something, you just measure it [laughs]! It was a bit of an eye opener to see just how slowly clinical research can progress compared with basic science. Another lesson was that to get clinicians involved you have to show them the carrot. You might say: “This is the research and if it’s successful it’s going to reduce the non-responder rate of breast cancer treatments by 80%.” At that point, their eyes will light up [laughs].