By Teresa Lemainque
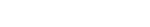
This MRM Highlights Pick interview is with Berk Silemek and Lukas Winter, researchers at Physikalisch-Technische Bundesanstalt (PTB) in Berlin, Germany. We chose to feature their paper entitled “Wirelessly interfacing sensor-equipped implants and MR scanners for improved safety and imaging” because they openly shared design files and software for the MRI implant sensor they developed.
MRMH: What’s your background and how did you get into MRI?
Berk: My background is in “EEE” (electrical and electronics engineering). Eight years ago, I started working as a research engineer at the National Magnetic Resonance Research Center (UMRAM) in Ankara, Türkiye, with Ergin Atalar, who introduced me to emerging MR hardware, parallel transmission (pTx) and implant safety concepts. I came to PTB to pursue my PhD, where Lukas served as my supervisor. My PhD project was part of a bigger EU project called MIMAS. Currently, I am involved in a continuation project called STASIS.
Lukas: I studied Electrical Engineering and Information Technology at the RWTH-Aachen in Germany, with a specialization in medical technology. My diploma thesis was on real-time neurosurgical robots and I worked at Siemens on Computed Tomography algorithms, so I had some imaging but practically no MRI experience during my studies. Nevertheless, I considered MRI such a cool technology, which wouldn’t bore me after 6 months, so I picked a PhD in ultra-high field MRI in Berlin, and I’ve never regretted it.
MRMH: Let’s turn to your paper. What was your goal behind this project?
Lukas: Our main motivation was, of course, to do some impactful research! In this particular case, we worked on an MR safety issue that exists for many years, namely the fact that implants can heat up in an MRI system. Currently the responsibility for patient safety lies with the clinical personnel. The workflow to guarantee safety is however very challenging and accidents can still occur even for MR conditional implants. Our vision is that implants like deep brain stimulators communicate with the MR scanner via an embedded sensor. The real cool thing about it is that the measured sensor data can be used to enhance both safety and imaging performance. Simultaneously! In the end, MR manufacturer and implant manufacturer would each have the responsibility for their device, taking the MR operator out of the equation. For the past few years, it was our research focus to demonstrate – step by step – how this can be done.
MRMH: What did you investigate in your research?
Berk: We established wireless communication between a custom-built reference implant and an MR scanner with the aim of getting relevant safety information from the implant tip during MRI. The reference implant mimics a deep brain stimulator. There are small low-cost sensors embedded in the implants electronics, which measure voltages from the electrode tip, where the maximum RF-induced heating occurs. In a calibration step with external probes, we determine how sensor voltages are related to E-fields and temperature changes. This allows us to know, within milliseconds, what is happening in the tissue during a scan. Furthermore, if we have two or more RF channels available, this information allows us to cancel RF-induced heating while maintaining image quality. This approach gives us the best of both worlds, imaging and safety!
Lukas: In a nutshell, we know from simulations of very complex, but realistic, geometries of implants that parallel transmission can substantially suppress RF-induced heating while maintaining image quality. However, if there is a slight modification in the setup, e.g., if we move the guidewire by only 1 cm, we may suddenly see heating rates double. This makes it really problematic to rely on simulations alone for RF pulse optimizations. Real-time information from the patient would be a big step forward and one way to get it is to use sensors. In the paper, we show that it is possible to use very cheap sensors to apply our methodology and that a communication between implant and MRI system is feasible. Many implants that are available as medical products already have sensors embedded that could be utilized. Both implant and MR manufacturers use Bluetooth protocols to communicate with external devices, so let the magic happen.
MRMH: That sounds great! How is your reference implant build up, and what quantities does it measure?
Berk: Deep brain stimulators come with a lead that has an uninsulated tip, which can heat up in an MRI scanner. These implants and implant leads are extremely expensive, and you cannot just buy them off the shelf! We’ve built a reference implant including both electronics and simple implant leads for this paper. The implant lead trajectories are based on realistic implant routing extracted from patient data that were openly shared in a publication. The electrode is connected to the casing, which contains our electronics, such as the sensor, signal sampling and processing units, a battery and a Bluetooth module including an antenna to send/receive data to/from an external server that communicates with the MRI system.
Lukas: By sending some low power RF pulses, you basically measure the impulse response at the implant. And from the aforementioned calibration step you know how the signal you measure corresponds to a safety relevant quantity, like temperature or SAR.

Teresa Lemainque: What components would I need if I were to start working on the same topic? A pTx system? Are these systems readily available?
Lukas: The reference implant is relatively easy to rebuild. All electronic parts are available online in the bill of materials that we provided. With the code that is shared you can start setting up some first experiments using wireless transmission. If you want to use pTx you may be surprised to learn that pTx systems — I mean the simplest ones — are fairly widely available, because the body coils of most modern 3T scanners can be driven by two channels. More channels would be better, of course, but such systems are still rare, unfortunately.
The research pTx system we used currently has sixteen transmission and four receive channels and has been published in 2020 in MRM (https://doi.org/10.1002/mrm.28379) alongside open-source design files and code for a rebuild. It’s a bit more expensive because of the component costs, but very flexible since it allows you to perform experiments over a wide frequency range (0.5T-7T). It works stand-alone but can also be hooked-up to an MRI system to perform imaging. Lastly you’ll need some RF coils. For easy reproducibility, we have published (https://gitlab1.ptb.de/) the design files for our 8-channel pTx RF coils for 3T and 7T.
MRMH: How far is the concept from real life? What steps are you taking to bring sensor-equipped active implanted medical devices closer to clinical practice?
Lukas: Let’s be realistic, right now, there seem to be few incentives for MR vendors to change the status quo, because the liability does not lie with them. Implant manufacturers have to perform heavy testing for implant safety to label their devices as MR conditional, but that is it. They specify the conditions but the clinical personnel needs to set these conditions at the scanner and is ultimately responsible.
However, what we are asking from the vendors is to sit down together and agree upon a practical implementation protocol. We are absolutely aware that it might be a huge and costly step, especially if products need to be partly redesigned. On the other hand, in the current approach, you need large safety factors and have to reduce power levels substantially, thus sacrificing image quality. Much better and safer imaging could be obtained when using a sensor-equipped implant. This will be an incentive for companies at some point. We are gathering more data to demonstrate that the proposed concept is feasible and also works with commercially available implants. Papers like this one will eventually be recognized by standardization working groups and regulatory bodies. This could motivate vendors to implement the concept and talk to each other. Besides providing such data and sharing our designs, we are working on uncertainties, communication workflow and risk-analysis and on test stands to calibrate the sensors. This is all happening within the EU project STASIS (https://www.ptb.de/stasis/) and will help to frame our concept. We are sharing our designs so that manufacturers or anyone else who’s interested could investigate these aspects alongside the methodology and help to translate it into clinical practice.

MRMH: What do you enjoy when you are not doing lab work on implants?
Berk: I try to play basketball twice a week, Lukas sometimes joins me, and I play a bit of chess.
Lukas: Spending time with my kids, yoga and meditation, cooking, dance… Many, many interests and little time for them all.
MRMH: How do you like your city, Berlin? Would you recommend it to international researchers?
Lukas: Definitely! Berlin probably has everything you might want, apart from mountains and the sea. There’s a nice vibe in the city, which I personally like very much. And so, I recommend coming to Berlin. By the way, we will be having a safety workshop in Berlin next year, so that might be a good opportunity.
MRMH: Berk, what does the immediate future look like for you?
Berk: I just defended my PhD thesis. At the moment, I’m continuing to work on the STASIS project.
MRMH: Congrats, and all the best! Thank you for the interview.